Valery Zolotov
Reading time: 4 minutes
A A
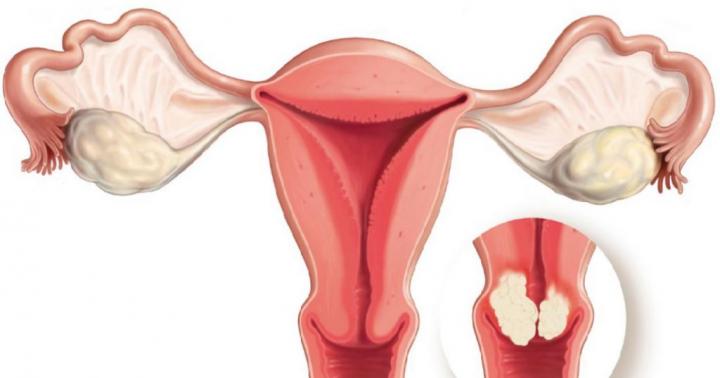
Blastoma is the general name for all tumors: benign and malignant. However, when it comes to cervical blastoma, we often have to talk about malignant neoplasms. Therefore, in this article we will consider a tumor of the cervix, ICD code 10 C53. We will tell you what it is, how to get rid of blastoma, and also how to prevent its occurrence.
Some general information
The international classification of diseases contains the code C53, which means a malignant neoplasm of the cervix. Statistics say that this is one of the most common cancers in women. Pathology is most often found in women of reproductive age. If this disease is detected in the early stages of development, the prognosis will be favorable. Otherwise, costly long-term treatment is in store.
The occurrence of a tumor is associated with the appearance of atypical cells with localization in the cervix. The natural cells of the endometrium are reborn, resulting in a malignant tumor. The disease progresses extremely rapidly, first infecting adjacent tissues and organs, and then distant ones. At the initial stage, the tumor is not dangerous to health.
At the moment, doctors distinguish four stages in the development of cervical blastoma. Each of them requires a special approach to treatment, has a different list of symptoms and consequences.
- Initially, a group of atypical cells is localized in the body of the uterus, here its primary development takes place. At this stage, there are no metastases yet, the patient feels good and may not even be aware that something is wrong in her body. At this stage, cancer is detected during a gynecological examination and instrumental examination.
- In the second stage, one can observe the growth of a malignant neoplasm in the cervix. There are still no metastases, but the tumor continues to progress and capture new territories. The first symptoms may appear: pain, bleeding. Often the disease and at this stage is asymptomatic.
- Now the blastoma extends beyond the uterus, affecting the pelvic organs and adjacent lymph nodes. Metastases spread to nearby organs, secondary cancerous tumors appear. At this stage, the treatment becomes much more difficult. It is necessary to remove the affected organs along with the formed tumors, to conduct a course of radiation therapy and chemotherapy.
- The fourth stage has the worst prognosis. The fact is that the tumor gives metastases even to distant organs. Sometimes it happens that secondary neoplasms affect vital, irreplaceable organs, then they become inoperable and therapy becomes symptomatic.
Why does a blastoma occur?
Benign and malignant blastomas occur almost according to the same scenario. As mentioned above, the appearance of atypical cells is to blame, but not everything is so simple. Mutating cells appear daily in the human body in large numbers. In a normal situation, the immune system successfully copes with them. However, she misses some of them. This is a real mystery for modern doctors. Nobody still understands why this is happening.
Next, I would like to talk about some risk factors. The more of them a person has, the more likely to get such a disease. In practice, it turns out that the majority of all women aged 30 to 35 are at risk. But that doesn't mean they're doomed. You just need to be more attentive to your health and undergo an examination by a gynecologist on time.
Now let's move on to the risk factors. If you have 2 or more of them, you need to be wary. It may make sense to change your lifestyle or visit a doctor for an examination.
- Frequent violations of the menstrual cycle, constant delays. Due to hormonal changes, imbalance of estrogen and progesterone, problems with ovulation are observed. The egg does not mature or does not come out at all.
- Infertility.
- Absence of children. Practice shows that women who have never given birth are more prone to developing cervical cancer. Moreover, the probability increases by about 2.5 times.
- Excessively long childbearing period. If menstruation began earlier and ended late, this means a strong long-term effect on the reproductive organs. As you know, prolonged mechanical impact on any human organ often leads to the formation of tumors.
- The onset of sexual activity before the age of 16.
- Overweight. Here, too, the problem lies in the production of hormones. Doctors have proven that the fatty layer contributes to increased production of estrogen. It is important to know that even a slight excess of the norm leads to an increase in the likelihood of developing a malignant neoplasm. Thus, an increase in weight by 10 kg from the norm increases the chance by 3 times, and by 25 - by 9!
- Long-term hormone therapy using estrogen. The longer, the more likely to get the disease.
- The presence of benign neoplasms in the body or in the cervix.
- Diabetes mellitus with insulin dependence. This disease also causes hormonal disruptions in the body.
- hereditary predisposition. If your close relatives have ever been diagnosed with cancer, then you are at risk.
- Chronic inflammatory diseases with localization in the uterus.
- Having bad habits. Alcohol and nicotine have a serious negative effect on the body and can increase the chances of developing cancer. Drug addiction is even worse. In addition, all these habits will not bring anything good to health.
- Promiscuous sex life and the presence of sexually transmitted diseases.
- Mature age. As mentioned above, the probability is increased in women from 30 to 35 years.
We remind you that all these factors are not a sentence. They only mean that you need to be more attentive to your health. In addition, many of these factors affect the likelihood of developing cancer in general, and not just malignant neoplasms in the cervix.
Symptoms
The localization of the neoplasm in the cervix gives its own unique symptoms, so it is quite easy for the patient to find out which organ the problem is with (but not in the first stages). But it is important to pay attention to the problem as soon as the signs have been detected.
Women who are at risk should visit a gynecologist regularly. The doctor, during a regular examination of the organs, is able to identify a neoplasm and send it for a more detailed study. Thus, a cancerous tumor is likely to stop bothering you after a short course of treatment.
The following symptoms may indicate a potential diagnosis: cervical cancer:
- bleeding not associated with menstruation;
- uncharacteristic discharge with an extremely unpleasant odor;
- blood after menopause;
- bleeding after any sexual intercourse;
- pain in the pelvic area during intercourse;
- constant pain that gets worse over time
- abrupt changes in the menstrual cycle;
- violation of the process of defecation and urination.
Features of treatment
Blastoma in the uterus is usually removed surgically. However, the choice always remains with the doctor. It all depends on the age and current condition of the patient. The size of the tumor, the degree of its ingrowth, the stage of the disease, the localization of metastases - all play a role in the choice of treatment. In addition to surgery, there are other methods of treatment:
- chemotherapy;
- radiation therapy;
- immunotherapy.
Of course, there are also experimental treatments, but it is too early to include them in this list, since their effectiveness has not been proven.
Surgery almost always means removing the tumor along with the uterus and its appendages. Yes, a woman is completely deprived of becoming a mother in the future. But otherwise, she remains a normal person and can continue life with the same level of quality. This is by far the best way to fight cancer. In some cases, it is also necessary to remove adjacent lymph nodes if parts of a malignant neoplasm are found in them.
Radiation therapy is used after surgery. It can be dispensed with only in cases where the removal of the blastoma was carried out at an early stage. Radiation therapy is designed to significantly reduce the likelihood of recurrence. Radiation affects only the affected area of the body.
Chemotherapy is used in combination with radiation and also reduces the chance of a tumor reappearing with the same localization. In any case, after the course of treatment, you will need to regularly visit a doctor to make sure that your health is normal.
|
What are the symptoms of intestinal blastoma? (Read in 3 minutes) |
In the structure of cancer incidence in women malignant tumors of the cervix account for almost 15% and among the lesions of the organs of the reproductive system consistently occupy the third place after breast cancer and endometrial cancer. In the structure of oncological mortality, cervical cancer also ranks third, second only to ovarian cancer and endometrial cancer. The disease is classified as "visual localization", while the quality of diagnosis does not improve. In Russia, initial cancer is detected in 15.8% of primary patients, advanced cervical cancer stages III-IV - in 39.5% of cases.
ICD-10 CODE
C53 Malignant neoplasm of the cervix.
EPIDEMIOLOGY OF CERVICAL CANCER
Every year, 370,000 primary patients with cervical cancer are registered in the world and 190,000 women die from this disease.
Most cases of cervical cancer (78%) occur in developing countries, which corresponds to 15% of all malignant neoplasms. It is the second most common cause of death. In developed countries, cervical cancer accounts for 4.4% of all malignant neoplasms, in Russia - 5.1%. The incidence for 10 years has slightly decreased from - 57.6% to 51.3% (in 2003). The peak incidence occurs at the age of 40–50 years. In young women in the age group up to 40 years, an increase in incidence rates is noted. Especially noticeable is the trend towards an increase in the number of cases of cervical cancer in people under 29 years old - 7% per year. This indicates both a low level of health education among the population, and insufficient attention paid to the treatment of background and precancerous diseases of the cervix in risk groups. Gynecologists of the general medical network have practically no oncological alertness during the examination of young women. The fact of an increase in the number of cases in this age group is considered a direct reflection of the low level of sexual culture of the population, associated with the lack of proper information about the role of contraceptives in the prevention of STIs.
PREVENTION OF CERVICAL CANCER
The risk of cervical cancer is highest in women of the promiscuous group (early onset of sexual activity, frequent change of sexual partners, presence of STIs, first birth at a very early age, frequent abortions). The main way to prevent cervical cancer is the timely detection of background, especially precancerous, processes and their treatment. Equally important is the use of barrier contraceptives that prevent the spread of STIs, which include HPV, which is considered an etiological factor in the development of cervical cancer. The treatment of HPV infection currently used cannot be considered completely satisfactory, since the approaches used are devoid of antiviral specificity and consist of immunotherapy and local impact (destruction, removal) on the lesion. Currently, vaccination [human papillomavirus vaccine (Gardasil®)] is effective in preventing HPV types 6, 11, 16, and 18-induced genital cancers, precancerous epithelial dysplasia, and genital warts.
SCREENING
The use of screening programs for examining the population makes it possible to detect the disease at the stage of precancer or in the initial form of cancer. A decisive role in making an accurate diagnosis is the correct conduct of diagnostic manipulations. The leading diagnostic screening test for mass examinations of the population is a cytological examination of smears from the cervix and cervical canal, which makes it possible to suspect pathological changes in the cervix in women of any age group. The Papanicolaou diagnostic method has become widespread abroad. In our country, one of the modifications of this method is used (staining smears with hematoxylin and eosin). The material for cytological examination is obtained from the zone of transitional epithelium in such a way that it contains cells not only of the superficial, but also of the deep layers. Before taking a smear, the cervix should be lightly wiped with cotton wool, slides should be degreased. The resulting material is transferred to the glass, carefully controlling the distribution of the material and making sure that the thickness of the smear is moderate. It should be remembered about the possible errors encountered at various stages of the cytological study:
- pathological cells do not fall into the scraping;
- the spatula does not capture the affected area;
- pathological cells do not fall from the spatula onto the glass slide;
- erroneous interpretation of the cytological picture.
The sensitivity of the method for cervical cancer is 85–95%.
Cervical cancer screening should begin 3 years after first sexual contact, but no later than 21 years of age. Screening frequency: annually for the first two years, with negative results every 2–3 years thereafter. Stopping screening is possible in women after 70 years of age with an intact cervix and on the condition of three or more registered, consecutive negative cytological studies within the last ten years.
CLASSIFICATION OF CERVICAL CANCER
Two classifications of cervical cancer are used in the world: according to the FIGO system (International Federation of Obstetricians and Gynecologists) and according to the TNM system, in which the prevalence of the lesion is recorded on the basis of a clinical study that includes all types of diagnostics (Table 29-1).
The zero stage of FIGO corresponds to CC Tis according to the TNM system - preinvasive carcinoma.
Table 29-1. Classification of cervical cancer. primary tumor
| TNM stage | FIGO stage | Characteristic |
| TX | Primary tumor cannot be assessed | |
| T0 | No obvious signs of a primary tumor | |
| Tis | 0 | Carcinoma in situ |
| T1 | I | Carcinoma of the cervix is limited to the uterus (there is no transition of carcinoma to the body of the uterus) |
| T1A* | IA | Invasive cancer diagnosed only microscopically. Stromal invasion with a maximum depth of no more than 5 mm, horizontally - no more than 7 mm. Involvement of blood or lymph vessels does not affect indexing |
| T1A1 | IA1 | Measurable stromal invasion up to 3 mm, horizontal spread up to 7 mm |
| T1A2 | IA2 | Invasion of the cervical wall more than 3 mm, but less than 5 mm, horizontal extension up to 7 mm |
| T1B | IB | Clinically detectable lesion limited to the cervix or microscopic lesion greater than T1A/IA2 |
| T1B1 | IB1 | Clinically detectable lesion up to 4 cm in maximum dimension |
| T1B2 | IB2 | Clinically detectable lesion greater than 4 cm in maximum dimension |
| T2 | II | Cancer spreads beyond the cervix, but without involvement of the pelvic walls and lower third of the vagina |
| T2A | IIA | Tumor without parametrial infiltration |
| T2B | IIB | Tumor with parametrial infiltration |
| T3 | III | The tumor infiltrates the parametrium to the walls of the pelvis and (or) the lower third of the vagina is involved and (or) causes hydronephrosis or dysfunction of the kidney |
| T3A | IIIA | The lower third of the vagina is involved in the tumor process, but the tumor does not spread to the walls of the pelvis |
| T3B | IIIB | Tumor invades the pelvic wall and/or causes hydronephrosis or obstructs the kidney |
| T4 | IVA | The tumor process involves the mucous membrane of the bladder or rectum and (or) the tumor extends beyond the pelvis |
* All macroscopically detectable lesions, even those with superficial invasion, are classified as T1b/IB.
With cervical cancer, the lymphogenous path of metastasis predominates, regional metastasis zones: external and internal iliac, obturator, common iliac, lumbar para-aortic lymph nodes (Tables 29-2, 29-3).
Table 29-2. Classification of cervical cancer. Damage to regional lymph nodes
Table 29-3. Classification of cervical cancer. Distant metastases
HISTOLOGICAL TYPES OF CERVICAL CANCER
The histological structure of the tumor is one of the most important criteria when choosing a treatment plan and for the prognosis of the disease. In most cases, a squamous cell form is detected (85% of cases), and among them, taking into account the degree of differentiation, keratinizing cancer (mature form) is 20–25%, non-keratinizing cancer (average degree of maturity) - 60–65%, poorly differentiated cancer (immature form) - 10–15%. In the endocervix, adenocarcinoma is relatively often detected - 15–20%. Rare forms of cervical cancer (clear cell, mucoepidermoid, small cell, etc.) are detected in 1–1.5% of patients.
ETIOLOGY (CAUSES) AND PATHOGENESIS OF CERVICAL CANCER
The leading role in the carcinogenesis of cervical cancer is assigned to PVI as the most common type of STI. The causative agent of PVI is a group of DNA-containing viruses belonging to the Papavaviriade (HPV - human papilloma virus) family, which have the ability to infect and transform epithelial cells of the cervix. With the help of molecular biological methods, about 100 HPV serotypes are identified, of which 30 are detected in lesions of the genital organs. There are the following forms of genital PVI: clinical, subclinical, latent. High oncogenic risk viruses include HPV types 16, 18, 31, 33, medium risk - types 30, 33, 35, 39, 45, 52, low - types 6, 11, 40, 44, 61. With squamous cervical cancer, most often HPV type 16 is detected, while type 18 is most common in adenocarcinoma, low-grade cervical cancer. Viruses of "low" oncological risk are detected mainly in genital and flat warts, mild dysplasia, and rarely in invasive cancer. Viruses of "high" oncological risk are found in 95-100% of non-invasive and invasive forms of cervical cancer.
The average age at stage I of cervical cancer is 47.6 years, at II - 57.7, at III - 55.9, at IV - 59.8 years. The ratio of detected stages of cervical cancer is as follows: stage I - 37.9%, stage II - 32.1%, stage III - 25.7%, stage IV - 4.3%. About 30% of patients with invasive forms of cervical cancer are young women.
CLINICAL PICTURE (SYMPTOMS) OF CERVICAL CANCER
CC belongs to tumors that are asymptomatic for a long time. The appearance of clinical symptoms and complaints indicates a far advanced tumor process. Most often, patients complain of profuse leucorrhoea, spotting and pain.
The first symptoms of cervical cancer. Whites are liquid, watery in nature and are caused by lymphorrhea from the site of the tumor, which has undergone necrosis or decay.
Bleeding is the most common clinical symptom. Bleeding in cervical cancer are in the nature of repeatedly randomly repeating spotting, aggravated in the premenstrual and postmenstrual periods. At the beginning of the disease, spotting is often in the nature of contact, occurs after intercourse, straining or digital examination of the cervix.
Pain in nature, localization, intensity are different, are localized in the lumbar region, sacrum and under the bosom.
Late symptoms of cervical cancer. They develop as a result of regional metastasis, germination of neighboring organs, and the addition of an inflammatory component. These include pain, fever, the appearance of edema of the limbs, disruption of the intestines, urinary system.
Common symptoms of cervical cancer. These include general weakness, increased fatigue, decreased performance.
DIAGNOSIS OF CERVICAL CANCER
ANAMNESIS
When clarifying the anamnesis, it is necessary to pay attention to past diseases, menstrual and reproductive disorders, changes in the functioning of the intestines and bladder, the age of the patient, marital status, lifestyle.
PHYSICAL EXAMINATION
The cervix is available for visual and invasive research methods, which helps to identify cervical cancer in the early stages. Early diagnosis involves several different studies.
Extended colposcopy allows you to study the state of the epithelium of the cervix under 7.5-40 times magnification. Particular attention is paid to the transformation zone. To increase the information content of the study, a number of specific samples are used. One of them consists in the application of a 3-5% solution of acetic acid to the cervix, which makes it possible to assess the state of the terminal vascular network that feeds the epithelium of the cervix. Normally, the vascular network is represented by various-sized, gradually branching vessels in the form of brushes, panicles, bushes. After treatment with acetic acid, normal vessels are reduced. Vascular atypia is manifested by a chaotic arrangement of non-anastomosing vessels of a bizarre shape. They are highly convoluted, have a corkscrew or hairpin shape, etc. (arise as a result of the rapid growth of the epithelium, due to a delay in the development of the vascular network), when treated with acetic acid, atypical vessels do not contract. Vascular atypia is considered a much more suspicious sign of malignancy than areas of keratinized epithelium. Malignant processes are often accompanied by proliferation of blood vessels and changes in their structure.
Schiller's test is widely used (treatment of the cervix with 2-3% Lugol solution with glycerol ©). This test is based on the ability of mature glycogen-rich stratified squamous cells to stain dark brown. Often, only with the help of this test, it is possible to identify pathologically altered epithelium in the form of iodine-negative areas. A correctly assessed colposcopic picture allows you to identify the affected area and perform a targeted biopsy from a suspicious area for subsequent histological examination.
LABORATORY RESEARCH
As a tumor marker of squamous cervical cancer in the patient's blood serum, the level of specific Ag - SCC is determined. Normally, it does not exceed 1.5 ng / ml. In squamous CC, in 60% of cases, an increase in the level of tumor-associated AG is detected. It is believed that if the SCC is initially elevated (more than 1.5 ng / ml), especially in stages IB and IIB, then the likelihood of cancer recurrence increases by 3 times. The concentration of this marker above 4.0 ng/ml in newly diagnosed patients indicates damage to regional lymph nodes.
INSTRUMENTAL STUDIES
If you suspect a precancerous pathology or cervical cancer, it is necessary to carry out an in-depth diagnosis (biopsy of the cervix, curettage of the cervical canal). When performing a biopsy, a number of conditions must be observed:
- biopsy is performed after colposcopy. Biopsy should be performed in conjunction with cervical scraping, preferably with prior cervicoscopy to allow visual evaluation of the endocervix. These measures in the presence of cancer can help in determining the level of damage (invasion), and therefore, to develop the right treatment tactics;
- a biopsy should be done with a scalpel, since when using a conchotome, the material taken is deformed and, as a rule, it is not possible to obtain the required volume of underlying tissues;
- when performing a biopsy, it is necessary, if possible, to remove the entire suspicious area with underlying tissues (departing from its borders, without damaging the epithelial layer, while capturing the stroma of the cervix by at least 5 mm).
A special role is played by the correct interpretation of the morphological study carried out by the pathologist.
Histological examination is considered the final and decisive method for diagnosing cervical cancer, which makes it possible to determine the nature of morphological and structural changes.
The stage of cervical cancer is determined using ultrasound, radiography of the lungs, cystoscopy, irrigoscopy. According to the indications, CT and MRI are performed.
INDICATIONS FOR CONSULTATION OF OTHER SPECIALISTS
All patients with suspected cervical cancer should be consulted by an oncologist (oncogynecologist) for an in-depth examination.
When the diagnosis is established, a consultation is required with the mandatory participation of an oncogynecologist, a radiologist and a chemotherapist to develop a treatment plan. After referral for consultation or treatment to a specialized center, it is necessary to monitor the fate of the patient and the course of treatment.
TREATMENT OF CERVICAL CANCER
GOALS OF TREATMENT
In the initial stages of cervical cancer in women of young, reproductive age, organ-preserving treatment can be carried out, since the tumor is most often localized in the zone of transitional epithelium, and if the cervical canal is affected, in its lower and middle thirds. An isolated lesion of the upper third of the cervical canal is observed extremely rarely (2% of cases), which indicates the local nature of the tumor lesion, and the frequency of metastasis to the lymph nodes does not exceed 1.2%.
The main goal of economical operations is to cure a malignant tumor in compliance with the principles of oncological radicalism and with the preservation of reproductive function.
INDICATIONS FOR HOSPITALIZATION
Hospitalization is indicated for surgery, chemotherapy, radiation therapy, combined treatment, and in some cases for complex diagnostic studies. Radiation therapy and chemotherapy can be done on an outpatient basis.
SURGICAL TREATMENT OF CERVICAL CANCER
In CC stage IA1 (without unfavorable prognostic factors), in young, reproductive age, somatically burdened patients, a high cone-shaped amputation of the cervix can be performed. After this operation (within healthy tissues) strict dynamic observation is shown. Pap smears are done after 4 months, after 10 months, then annually, if both previous studies of oncological pathology have not revealed. In older people, hysterectomy is recommended.
With the prevalence of cervical cancer up to stage T1A2, the incidence of regional lymph node involvement increases to 12%, so pelvic lymph node dissection should be included in the treatment protocol. Recommend the Wertheim operation, or extended hysterectomy with ovarian transposition.
To preserve reproductive function, a high cone amputation of the cervix with retroperitoneal or laparoscopic pelvic lymph node dissection can be performed. Dynamic observation is carried out using Papanicolaou smears after 4 and 10 months, subsequently, in the absence of pathology in two smears, annually.
Standard surgical treatment of cervical cancer stage IB1: extended extirpation of the uterus with appendages.
In patients of reproductive age, the ovaries can be preserved and removed from the pelvis (postoperative radiation therapy is possible). Ovarian transposition can be performed in high- and moderate-grade squamous cell carcinoma and in the absence of tumor vascular embolism.
COMBINED TREATMENT FOR CERVICAL CANCER
In patients with early stages of cervical cancer (IB1, IIA<4 см) прогноз благоприятный. Заболевание может быть радикально излечено как с использованием хирургического метода в сочетании с брахитерапией, так и при использовании лучевой терапии.
The choice of treatment method depends on the age, somatic status, opinion of the patient. Treatment tactics are determined at the consultation. The patient should be informed about therapeutic alternatives, including complications and expected outcomes. Standard radiotherapy in stages IB1 IIA (tumor<4 см в диаметре): дистанционное тазовое облучение в сочетании с брахитерапией. Рекомендуемые дозы, включая дистанционную и внутриполостную радиацию, составляют 55–65 Гр. Доза дистанционного компонента на область таза должна быть 40–45 Гр. Соответственно дозы при брахитерапии необходимо определять согласно биологической эквивалентности.
Primary treatment for stage IB2–IIA cervical cancer (primary >4 cm in diameter) includes
- chemoradiotherapy;
- extended hysterectomy and postoperative radiation (chemoradiation) therapy;
- neoadjuvant chemotherapy (three courses of chemotherapy based on platinum drugs), accompanied by extended hysterectomy, with the addition of postoperative radiation or chemoradiotherapy, if indicated.
Chemoradiation treatment. A combination of external beam radiation therapy and intracavitary radiation therapy with parallel chemotherapy based on platinum preparations (fluorouracil in combination with cisplatin or cisplatin alone) is recommended for use. The total doses of radiation exposure should be 80–85 Gy, at point B - 50–65 Gy.
Extended extirpation of the uterus and postoperative radiation (chemoradiation) therapy. With extended hysterectomy, at the first stage it is possible to clarify the extent of the tumor and prognostic factors (presence of vascular embolism, severity of invasive growth, involvement of regional lymph nodes). After the operation, combined radiation or chemoradiotherapy is performed. The risk of recurrence is higher in patients with lymph node involvement, large tumor volume, perivascular and vascular invasion, and deep infiltrative growth greater than one third of the cervical wall. Adjuvant radiotherapy to the pelvic area improves survival rates compared to surgical treatment alone. The use of adjuvant chemoradiotherapy (fluorouracil in combination with cisplatin or cisplatin alone) when a tumor is detected in the resection margin improves patient survival compared to the standard variant of radiation exposure.
Neoadjuvant chemotherapy combined with extended hysterectomy. The treatment option for stage IB2-IIA cervical cancer (tumor >4 cm in diameter) is considered to be three courses of preoperative chemotherapy (platinum-based regimens) followed by extended hysterectomy, postoperative radiation or chemoradiotherapy.
The complication rate with combined treatment is higher than with surgery alone.
A reduction in the risk of complications without worsening oncological results is facilitated by a slight decrease in irradiation fields, including the vagina, parametrium tissues with an upper border located at the level of S1–S2, and not at the level of L5–S1 vertebrae.
In locally advanced cervical cancer (stages IIB, III: parametric, vaginal, and IVA), primary treatment includes external beam radiation therapy, brachytherapy, and chemotherapy. In the case of high efficiency of such exposure, it is possible to perform the Wertheim operation with subsequent continuation of radiation therapy (taking into account previously received doses). Patients of reproductive age may undergo ovarian transposition prior to the start of special treatment in order to maintain hormonal homeostasis.
Primary pelvic evisceration is performed at stage IVA cervical cancer, provided there is no damage to the pelvic wall, vesicovaginal or rectovaginal fistula. In the second stage, chemoradiotherapy is recommended.
Treatment of cervical cancer stage IVB and relapses is considered the most difficult. The prognosis is usually unfavorable. Relapses are divided into pelvic, distant and mixed. Most of them develop within the first 2 years after confirmation of the diagnosis. The average life expectancy is 7 months.
Treatment of local recurrences includes various surgical approaches: from the removal of the actual recurrent tumor, up to pelvic evisceration. Radical irradiation with adjuvant chemotherapy is indicated for isolated recurrence after radical surgery.
With the appearance of metastases in the pelvis or with continued growth of the tumor after non-radical treatment, chemotherapy is performed with a palliative purpose. Cisplatin is considered the most effective drug for the treatment of cervical cancer.
The average life expectancy in this case is up to 7 months.
Treatment options for local recurrence after radical radiotherapy may include extended extirpation of the uterus with appendages or pelvic evisceration (depending on the extent of the tumor). Extended resections are indicated in patients with "central" localization of recurrence, involvement of the bladder and (or) rectum, without signs of intraperitoneal or pelvic extension, without involvement of the pelvic walls in the process.
The prognosis is relatively favorable in patients who have undergone complete remission for more than 6 months, in whom the size of the recurrent tumor is less than 3 cm in diameter, and the side walls of the pelvis are not involved. The five-year survival rate after pelvic evisceration is 30–60%; operative mortality does not exceed 10%.
In patients with stage IVB cervical cancer and when metastases are detected, systemic chemotherapy plays a leading role in the treatment.
Typically, cisplatin-based regimens are used.
Local radiation exposure to distant metastases is used to achieve a palliative effect in pain syndrome due to damage to the bones or brain.
FURTHER MANAGEMENT
Periodic examinations of patients from the 3rd clinical group should include: assessment of complaints, general and gynecological examination, cytological examination of smears from the cervical stump and from the cervical canal after organ-preserving treatment or from the vagina. It is necessary to determine the dynamics of the expression of tumor markers (SCC), ultrasound, and, if indicated, CT at intervals of 1 time in 3 months during the first two years, 1 time in 6 months for 3, 4 and 5 years or until signs of progression are detected. A chest x-ray should be done every 6 months.
FORECAST
The survival of patients is directly related to the stage of the disease, and its five-year indicators are: for stage I - 78.1%, II - 57.0%, III - 31.0%, IV - 7.8%, all stages - 55.0 %. The five-year survival rate of patients with cervical cancer after combined treatment reaches high values, which is associated with the improvement of treatment methods, as well as with the observance of the principles of a differentiated approach to the choice of treatment method. However, the degree of spread of cervical cancer remains one of the main prognostic factors. In this regard, improvements in treatment outcomes are achieved mainly by increasing the life expectancy of patients with stage I and II cancer, while those in stage III remain stable.
Uterine cancer is the most dangerous cancer in women. Recently, unfortunately, experts have recorded an increase in the spread of this pathology, which causes great concern. Like any oncology, pelvic neoplasms have a good prognosis for cure if they are detected at an early stage. A neglected disease leads to tragic consequences. That is why any woman should conduct periodic preventive examinations to identify pathological problems as early as possible.
Essence of pathology
Uterine cancer - what is it? At its core, this is a hormone-dependent malignant formation that can metastasize to another formation in the pelvis or spread to other organs. This oncological form is considered one of the most common in women, second only to lesions of the breast, colon and lungs. It also occupies a fairly high place in terms of deaths with neglect of the disease. Most often, education in the uterus is recorded in women over the age of 45-48 years, but young women are not immune from it.
What is a uterus? This is a hollow-type organ 7.5-10 cm long and up to 5.5 cm wide in the area of the fallopian tubes with a thickness of up to 3.5 cm. The body and neck are clearly distinguished in the structure of the uterus, connected by a small, narrow passage. The uterine wall is covered with 3 layers: outer (serous), middle (myometrium, muscle layer) and inner, mucous (endometrium). In women of reproductive age, the endometrium is periodically rejected, coming out with menstruation. The manifestation of malignancy can be found in any of these elements.
Taking into account the localization of the lesion, an international classification according to ICD-10 can be given:
- common code - uterine cancer: bodies - C54, cervix - C53;
- code for localization of the tumor in the uterine body: isthmus - C54.0; endometrium - C54.1; myometrium - C54.2; uterine fundus - C54.3; other lesions of the body, C54.8;
- code for the localization of education in the cervix: internal cavity - C53.0; outer surface - C53.1; other lesions C53.8.
When a malignant tumor develops, uterine endometrial cancer is most often detected.
This was the reason that this type of pathology often becomes synonymous with the common name of uterine cancer.
How is pathology classified?
In world oncological practice, a division of the diseases under consideration is used according to the FIGO method (developed by the International Federation of Gynecologists) and the TNM system, which takes into account clinical manifestations identified by various diagnostic methods. According to morphology, cancer in the uterus is classified into the following forms: fibroids, adenocarcinoma; clear cell adenocarcinoma; squamous, glandular squamous, serous, mucinous and undifferentiated cancer.
Taking into account the mechanism of formation growth, the following varieties are distinguished: with a predominance of an exophytic character; with a predominant endophytic mechanism; mixed (endoexophytic) form.
An important factor of malignancy is the degree of tumor differentiation, and the lower this degree, the more dangerous the development of pathology. The characteristic is set in relation to the level of cells of the undifferentiated type. Uterine cancer is classified into the following categories:
- highly differentiated (G1);
- moderately differentiated (G2);
- poorly differentiated (G3).
According to the clinical picture, the following stages of uterine endometrial cancer are distinguished:
- the first stage: the formation in the uterine cavity is within the inner layer, while a slight germination into the muscle layer is possible;
- second stage: in addition to the defeat of the uterine body, there is a formation on the cervix;
- third stage: near metastasis begins, resulting in a tumor of the small pelvis in women (spread goes to the vagina, pelvic and lumbar lymph nodes);
- fourth stage: multiple metastases develop - spread, rectum, liver, lungs.
Etiology of the disease
A completely etiological mechanism for the appearance of a malignant tumor has not yet been identified. Researchers agree that it is associated with a violation of hormonal homeostasis as a result of functional lesions in the hypothalamus and pituitary gland, causing hyperplastic type processes due to proliferative changes in the endometrium. This process provokes malignant neoplasia.
The following causes that can cause a cancerous tumor are distinguished:
- Pathologies of the endocrine type: diabetes mellitus, hypertension, obesity.
- Damage to the genital organs with a change in their hormonal functions: hyperestrogenism, anovulation, female infertility, fibroids.
- , especially cellular granulosa tumor and Brenner's disease.
- Hereditary predisposition at the genetic level.
- Abnormal course of pregnancy or childbirth, excessively long absence of sexual relations, absence of childbirth.
- Too late onset of menopause - over the age of 54-56 years.
- Uncontrolled hormone therapy, including the use of Tamoxifen.
Disease pathogenesis
There are several theories about how uterine cancer develops. Almost 2/3 of cases are associated with the estrogenic mechanism of the development of the disease, when hyperestrogenism manifests itself in conjunction with endocrine and metabolic disorders. In these cases, the following processes are characteristic: uterine bleeding, hyperplastic phenomena in the ovaries, the conversion of androgens into estrogens in fatty tissues. With the estrogenic mechanism of the development of pathology, the nascent formation of the uterine body, as a rule, refers to a highly differentiated tumor with slow growth and weak metastasis.
Another variant of the development of the disease does not depend on estrogens. In almost 1/3 of patients, a malignant tumor of the uterus progresses against the background of endocrine disorders and the absence of ovulation. Atrophy of the endometrium occurs, which leads to tumor processes. Such oncology has low differentiation and is very dangerous by the rapid growth of the tumor.
Finally, the third theory is based on the development of neoplasia, which is caused by birth defects.
The volumetric development of a malignant tumor goes through several characteristic stages:
- At the first stage, functional changes are detected in the form of hyperestrogenism, anovulation, etc.
- The second stage is characterized by the formation of auxiliary morphological structures: polyps, cystic manifestations, benign fibroids.
- The third stage implies the appearance of precancerous structures, in particular atypical hyperplasia with epithelial dysplasia.
- At the fourth stage, malignancy of cells occurs directly with the development of cancerous neoplasms. The following sub-stages are distinguished: pre-invasive formations, fibroids with a slight ingrowth into the muscle layer, a pronounced oncological form of the endometrium.
Symptomatic manifestations
What does uterine cancer look like? The manifestation of the disease at different stages varies from complete lack of expression to unbearable pain in the last stage. At the initial stage of the formation of a neoplasm, the symptoms are almost invisible. The first real signs of cancer can be detected by vaginal discharge of a bloody nature, significant watery leucorrhea and pain of moderate intensity.
The most common symptom of uterine cancer is atypical uterine bleeding. However, this symptom immediately causes anxiety in postmenopausal women, when there should be no discharge at all. In reproductive age, such a symptom does not immediately cause concern, since it sometimes refers to minor gynecological disorders. This often leads to misdiagnosis of the disease.
Another important symptom is profuse serous discharge or leucorrhoea. They are also especially alarming for older women. This symptom is characteristic of both uterine body cancer and cervical cancer. Severe pain syndrome is an indicator of the neglect of the disease. It acquires an intense cramping character of an almost constant type as the disease progresses. Pain is especially sensitive in the lower abdomen and lumbosacral area.
We should also not forget about the symptoms of a general nature: weakness, fatigue, sudden weight loss. Women develop infertility and ovarian dysfunction.
Principles of treatment of pathology
Intensive treatment of uterine cancer begins with an accurate and definitive diagnosis. The first data on the presence of the disease give the results of ultrasound. More voluminous studies are performed on tissue samples obtained by biopsy. Histological methods allow you to get a complete picture of the presence of a tumor, its size and the stage of development of the pathology.
The most effective way to treat cancer is surgery. Even in the early stages of the disease, to exclude relapses, as a rule, the complete removal of the uterus, fallopian tubes, ovaries and nearby lymph nodes is carried out. Such a radical method eliminates errors in determining the size of the lesion. Lymphadenectomy, including excision of the external and internal iliac lymph nodes, can significantly reduce the risk of residual metastases.
The combined pathology treatment regimen includes such potent technologies as radiation exposure and chemotherapy. Radiation therapy is based on the effect of ionizing radiation on the affected tissues. Most often, it is used after a surgical operation to eliminate possible areas of regional metastasis. The degree of exposure is determined individually, taking into account the characteristics of the female body and the condition of the patient.
Chemotherapy is based on the use of potent chemicals that kill transformed cells. In the case of uterine cancer, this technique is used quite rarely. Sometimes, according to the decision of the doctor, drugs Cisplatin, Doxorubicin, Cyclophosphamide are prescribed.
Complex treatment also includes hormone therapy. It is most often provided with gestagens, antiestrogen and combined agents. At an early stage, a solution of hydroxyprogesterone caproate is usually prescribed. As the disease progresses, the doses of the drug are increased or other drugs are prescribed, such as Medroxyprogesterone. In addition, modern hormonal preparations of the 2nd and 3rd generations are actively used.
Cancer in the uterus is a fairly common cancer. It must be detected in the early stages, although diagnosis during this period is greatly hampered by the asymptomatic course of the disease. Advanced stages of pathology have a pessimistic prognosis and often lead to death.
Uterine cancer
3.3 (65%) 4 rating[ok]In the ICD-10, it is classified as a malignant neoplasm. In the case when the tumor is localized inside, then its code in the ICD is C53.0, and outside - C53.1. With lesions of the cervix that go beyond one or more of these localizations, it is assigned the code C53.8. Such a classification is not considered clinical and does not affect the choice of treatment.
Statistics
Among all types of oncological pathologies of the female genital area, cervical cancer is approximately 15% and ranks 3rd after malignant neoplasms of the endometrium and breast. This diagnosis annually claims the lives of more than 200,000 women worldwide. In Russia, this type of oncology ranks 5th among the causes of death in women from malignant tumors. In recent years, this oncological pathology has become most often determined in women under the age of 40 years.
Individual approach to treatment
Doctors adhere to the standards of cervical cancer treatment (according to ICD-10 - C53), using innovative methods of surgical interventions, radiation treatment and the most effective anticancer drugs. At the same time, an individual approach to the choice of the method of therapy for each patient is extremely important. The use of modern diagnostic techniques, therapy, including surgical methods, immunotherapy, chemotherapy, radiation allows oncologists to increase the survival rate of sick women.
Reasons for development
At the moment, scientists have not established factors that provoke the development of cervical cancer (according to ICD-10 - C53). It is believed that oncological processes develop under the influence of various causes. Viral infections, chemical effects on the female body, mechanical damage to the tissues of the cervix are considered exogenous.

The following endogenous factors in the development of such a pathological process are distinguished:
- hormonal imbalance;
- genetic predisposition;
- metabolic disorders;
- decrease in the immune resistance of the female body.
HPV
In 90% of cases, the triggering cause of this disease is HPV. Most often, a malignant tumor causes 16, 31.18, 33 types. Usually, a type 16 virus is detected in cervical cancer. Its oncogenicity increases significantly with a decrease in the body's immune response. The virus, which is involved in the mechanism of the onset of pathology, is transmitted through sexual contact. In most cases, spontaneous recovery occurs. But if pathogenic microorganisms in the cervix stay constantly, a cancerous tumor develops.
chronic inflammation
Significant factors provoking the development of pathology include the inflammatory process of a chronic course. It leads to the formation of dystrophic changes in the structures of the epithelium of the cervix, which ultimately causes the development of severe complications. An equally important factor in the development of oncology of this kind is traumatic injury during abortion, during childbirth, as well as some contraceptives.

Exogenous and endogenous factors
To exogenous causes of cervical cancer (according to ICD-10 - C53), experts include early sexual activity with various sexual partners, as well as smoking. The following endogenous factors are distinguished:
- increased levels of estrogen in the blood;
- immunodeficiency states in women, including the presence of HIV infection;
- prolonged use of oral hormonal contraceptives.
Do not forget about a variety of occupational hazards, quality and lifestyle.
Symptoms of the disease

At the beginning of the process of its formation, cervical cancer (according to ICD-10 - C53) does not show any pathological signs that can greatly disturb a woman. Only when the malignant formation begins to disintegrate, the following pronounced signs appear:
- leucorrhea of a different nature;
- soreness, most often localized in the lower abdomen, in the back, and also in the rectum;
- bleeding that occurs with local, even fairly mild trauma as a result of ruptures of small, fragile vessels of tumor formation, located superficially.
An oncological tumor can metastasize through the lymphatic vessels into the walls of the vagina by sprouting in places of its contact with an oncological tumor. The ureter is most resistant to tumor growth. Much more often, specialists detect compression of the ureters by oncological infiltrates, as a result, the normal outflow of urine is disturbed.
The growth of a tumor in the rectum indicates the neglect of the oncological process. The mucous membrane of the rectum, as a rule, does not remain mobile over the tumor for a long time. Rarely, cervical cancer can spread to the ovaries and fallopian tubes. Metastases to distant tissues and organs in untreated cases are rare.
Gynecologists are of the opinion that cervical cancer most often remains a “local process” for a long time. Metastasis is extremely rare, which gives clinical symptoms of a general infection. The temperature in sick women is kept at high levels, sometimes giving periods of remission. Cancer cachexia is observed at a late stage of oncological tumor formation and is caused by various pathological complications.

Symptoms of cervical cancer (ICD-10 - C53) should not go unnoticed.
With the development of a malignant tumor, the entire neck or its individual sections appear to be dense to the touch, enlarged, the mucous membrane is thickened. Often, anomalies of the integumentary epithelium are visualized in places. Often you can see an excess of tissue in the form of whitish areas of various shapes and sizes.
What to do if cervical cancer is suspected (according to ICD-10, code C53)?
Diagnosis of pathology
At the moment, there is a variety of diagnostic methods. The basis for the diagnosis of cervical oncology is a complete examination of a woman, the correct collection of an anamnesis of life and disease and complaints, an adequate assessment of the severity of the patient's condition, a gynecological examination using mirrors. The following instrumental methods for diagnosing this disease are used:
- colposcopy;
- laboratory tests for STIs;
- taking material for a biopsy;
- cytological screening.
Colposcopy is considered one of the most effective methods for diagnosing both directly malignant cervical cancer (ICD-10 - C53) and precancerous conditions. The efficiency of this method reaches 80%. Oncologists combine it with other modern technologies. Colposcopy allows you to determine the depth and nature of damage to the cervix as a whole, the boundaries and dimensions of the affected area, in order to subsequently conduct some morphological studies.

Important in the diagnosis of pathology is cervicoscopy. This study is performed using a hysteroscope. This technique has some contraindications:
- pregnancy;
- inflammation processes;
- bleeding.
Cervicoscopy allows you to assess the clinical condition of the cervical canal and shows an increase of up to 150 times, due to which targeted biopsy is carried out. One of the effective methods for determining the location of the tumor is a cytological study, which is recognized worldwide and recommended by WHO. In combination with colposcopy, the effectiveness of this study reaches 90-95%. The essence of cytology is the collection of cells from the cervix and their microscopic examination in order to detect pathological elements. A decisive role in the diagnosis is assigned to the histological examination of the biomaterial obtained by biopsy.
Treatment
The choice of treatment for cervical cancer (ICD-10 code - C53) is determined individually. Therapy depends on the prevalence of the oncological process and the severity of comorbidities. The age of the woman is of the least importance. The traditional methods of treating the disease include:
- surgical;
- combined;
- ray.

At the moment, scientists are actively studying the possibilities of chemoradiotherapy for cervical cancer (according to ICD-10, code - C53) and drug therapy.
In severe intraepithelial cancer, diagnostic separate curettage of the uterus and conization of the cervix are performed using an electric knife, scalpel, or laser beam.
Currently, in the treatment of invasive cancer of the 1st and 2nd stage, extended extirpation of the uterus and appendages (Wertheim's operation) is used. Combined treatment involves radiation therapy and surgery in a different sequence.
For a simpler designation of the disease, an international classification of diseases was invented, which also includes oncological diseases. The ICD code 10 for uterine cancer is denoted C54.
Improved localization
- C54.0 Inferior segment or isthmus.
- C54.1 Endometrial cancer.
- C54.2 Myometrium
- C54.3 - The fundus of the uterus.
- C54.8 Body of uterus extending beyond the above areas.
- C54.9 Unrefined zone
Tumor of the female genital organs
This group includes all malignant neoplasms that are located in the female reproductive system.
- C51 - Vulva.
- C52 - Vaginas.
- C53 - Cervix.
- C54 - Body.
- C55 Unfinished zone of uterus.
- C56 - Ovaries.
- C57 - Unspecified localization of the female reproductive system of gynecology.
- C58 - Placenta.
In turn, this group is included in the higher system of formations C00 - D48.
Oncology
Cancer of the body or cervix - occurs as a result of a mutation of the epithelial cells of the mucous membrane of the organ, which causes a neoplasm with uncontrolled division, which germinates and destroys the nearest cells and tissues.
Causes and factors
Uterine cancer is more common in older women after the onset of menopause. But there are also special cases at a younger age in young girls.
- genetic predisposition.
- Refusal of sexual life.
- Infertility.
- Women who have never given birth after 25 years.
- Obesity and malnutrition.
- Smoking abuse, alcohol.
- Diabetes.
- Improper use of hormonal contraceptives and drugs.
With any hormonal imbalance in the female body, the soil arises for the development of hormone-dependent carcinoma.
Signs, symptoms, abnormalities
- Frequent fever, no other prominent symptoms.
- Severe pain in the abdomen.
- Later, the pain will begin to radiate to the lumbar region.
- Bloody or even purulent discharge from the vagina with an unpleasant odor. In this case, the blood can go outside the menstrual cycle.
stages

- Stage 1 - at the initial stage, the neoplasm is located in the endometrial zone and does not cross the conjunctival membrane.
- Stage 2 - the tumor can affect the cervical canal and intracervical glands.
- Stage 3 - defeat and metastasis to local lymph nodes, vagina and abdominal cavity.
- Stage 4 - metastases penetrate through the blood to distant organs.
Diagnostics
- Visual examination by a gynecologist.
- Biopsy of suspicious lesions.
- Abdominal ultrasound.
- MRI for a more detailed examination.
- Analyzes for tumor markers to track the dynamics of tumor growth and the quality of treatment.